Re-imagining the future of the waiting room to gain a holistic understanding of patients
Challenge
To explore the relationship and communication between physicians, patients, and caregivers and understand the difficulties that elderly patients with chronic diseases face to design an intervention that would empower them to better understand, implement, and manage their conditions at home.
Duration
7 months
Team
Suzanne Choi, Grace Cha, Dayne Chung
My role: Problem framing, Research and Strategy, Concept Development, Environment Design

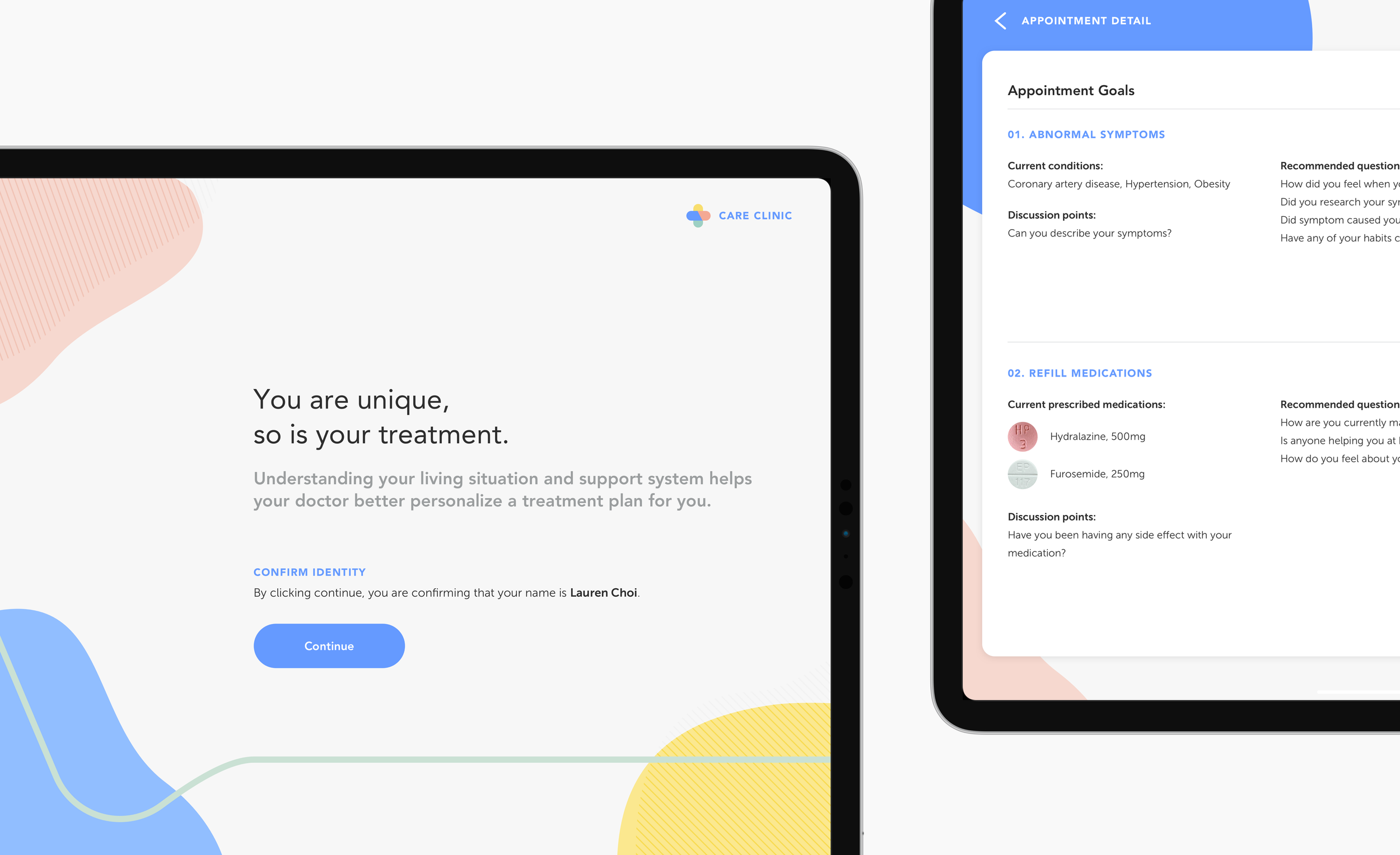
Care Clinic
Care Clinic is reimagining the primary care check-in process and waiting room environment. Care Clinic aims to provide an opportunity to gain a holistic view of the patient to improve patient-doctor communication, which affects the patient's receptiveness, attitude, and impression of the care they receive.
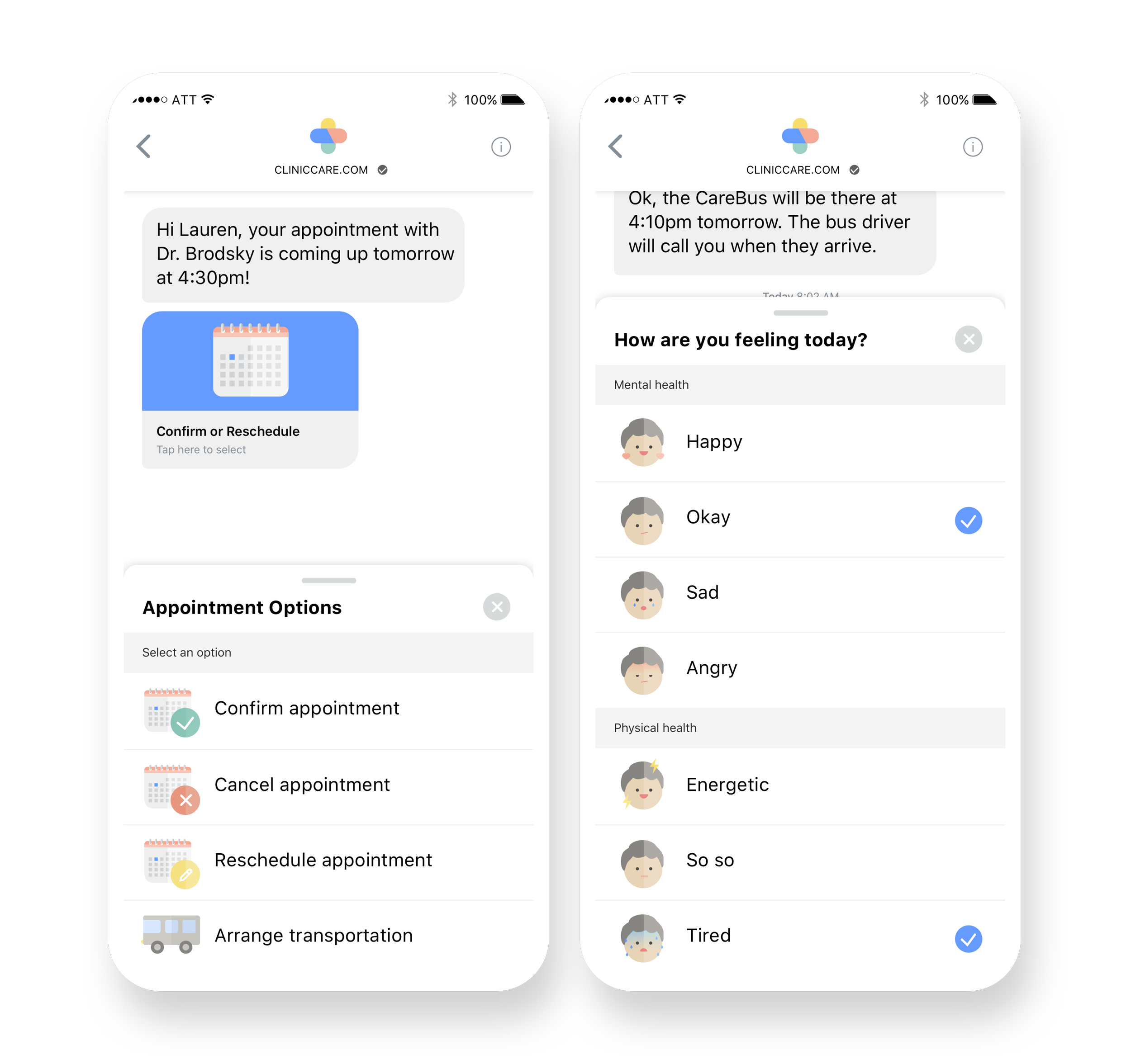
Easing the Process
CareText helps set a positive tone by reducing the stress of managing multiple administrative tasks, such as arranging transportation and rescheduling appointments.
The patient's emotional status is collected, enabling the clinic staff to tailor their approach to engaging with the patient to influence their receptivity to the doctor's recommendations.
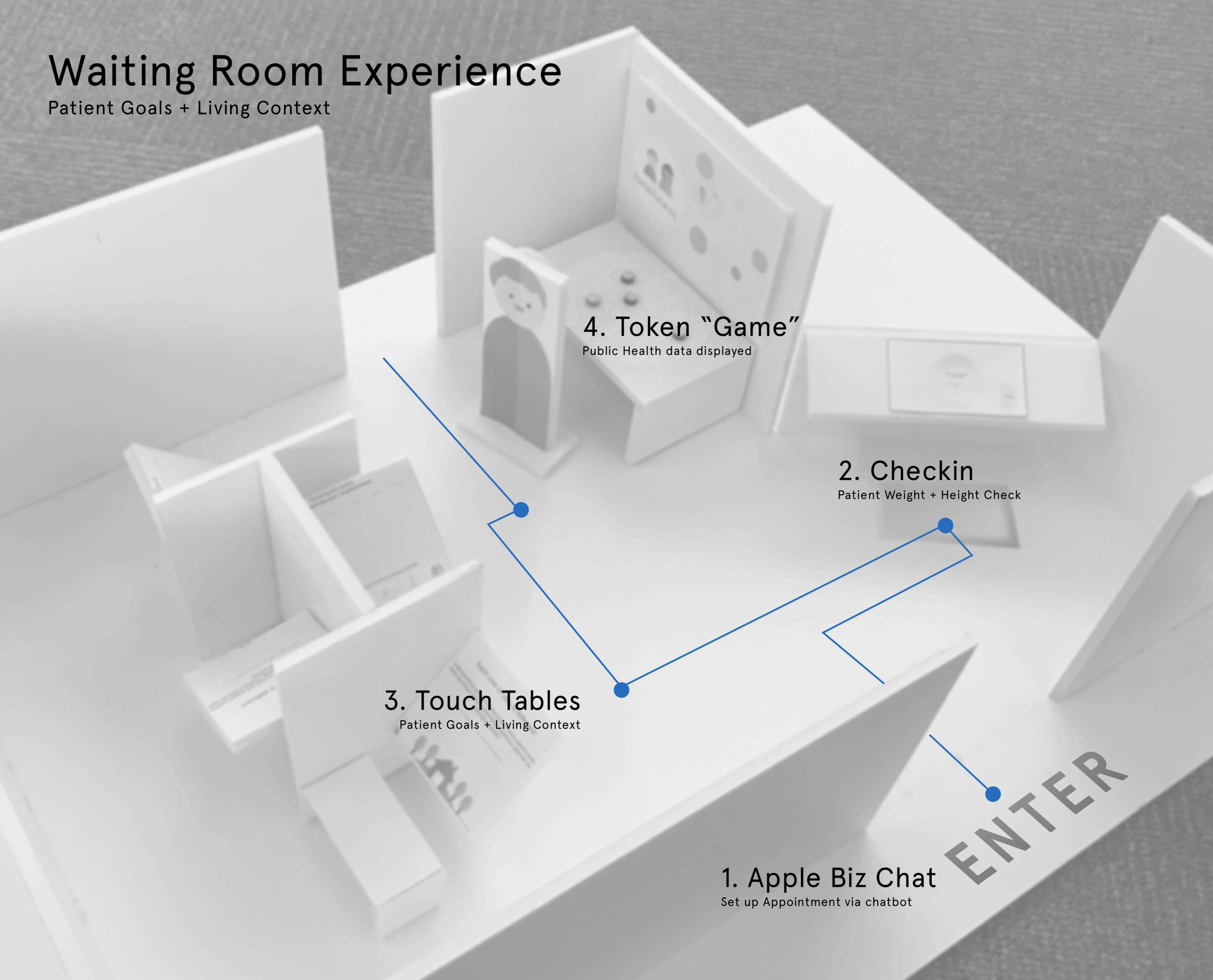
Streamlining the Journey
Rearranging the patient journey to use the check-in time more efficiently allows for in-depth conversations between the patient and health providers.
When the patient arrives, they scan their Care Clinic ID card, confirm their personal information, and have their vitals checked, all with the assistance of a Care Clinic health receptionist.
Gaining a Holistic Picture
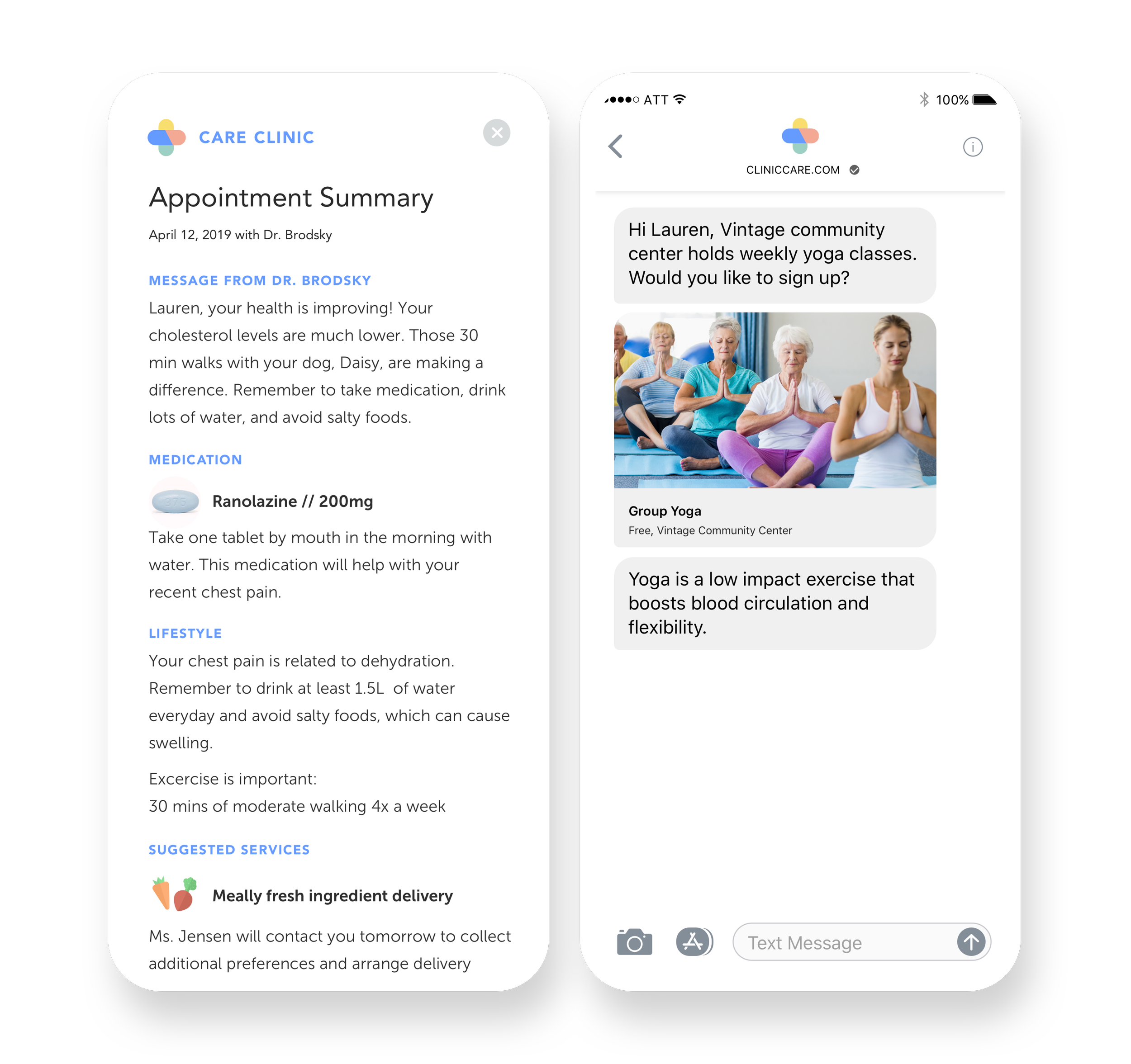
CarePad provides an opportunity to gain insight into a patient's living and social context.
With this information, the doctor can better personalize treatment plans based on a patient's capabilities and resource availability to increase patient motivation and treatment adherence.
The patient receives personalized service recommendations for greater autonomy in managing their condition at home.
Understanding Expectations
The patient can voice their expectations and priorities for the appointment and any personal concerns they want to discuss with their doctor.
With this information, the doctor can efficiently utilize the limited appointment time for a focused discussion and address the lifestyle burdens that may be mentally weighing on the patient.
Focus on Targeted Conversations
Based on the information collected, personalized patient discussion guides are generated that the doctor can use to have targeted conversations with the patient and build personal relationships.
Suggestions on resources and services for the patient help the doctor tailor treatment plans to the patient's capabilities and needs and promote them to encourage patients to find an appropriate support system when beneficial to treatment adherence.
Ongoing Support
Once home using CareText, the patient can review their discharge instruction, which incorporates personal messages and a summary of the discussion from the appointment in language based on the patient's cognitive ability and health literacy levels.
The patient receives continuous support between appointments through personalized recommendations and information based on the patient's profile.
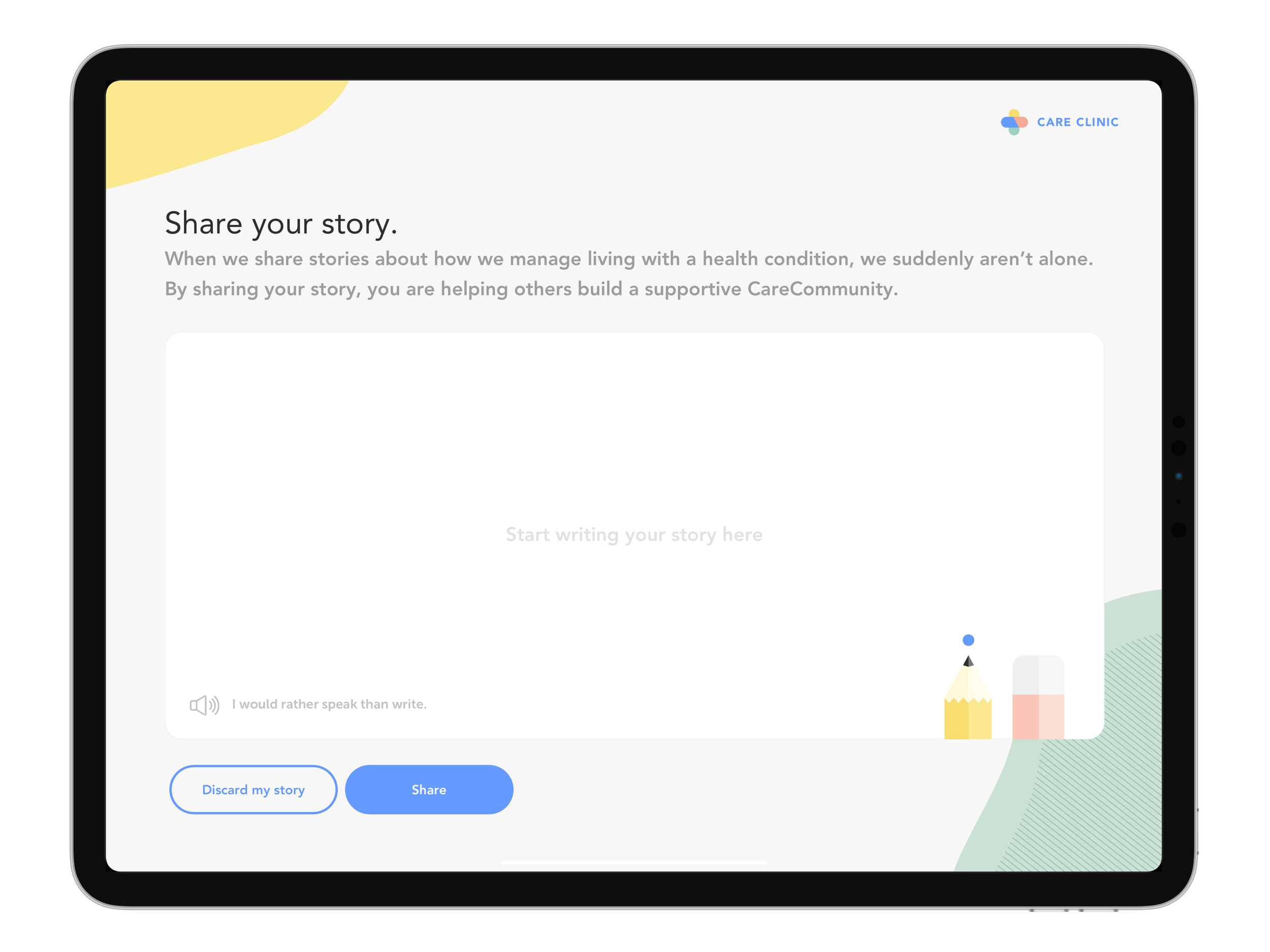
Sharing is Caring
Care Clinic is a welcoming space that promotes social interactions and influences a positive attitude in patients.
Care Wall is a space for patients to voice their personal experiences to build a supportive patient community. These stories provide emotional support by helping others see they are not alone in this journey.
Once the patient shares their story, it will appear anonymously on the wall on a delay, inviting patients to comfortably share their feelings and experiences without worrying about being identified.
So, how did we get here…read more about the process below
The Big Question
How might we help elderly patients with chronic conditions better understand and manage their treatment plans at home?
Research
To tackle this challenge, we conducted market research and expert and patient interviews. We broke down our initial questions to help us contextualize the experience of elderly patients who had a range of chronic conditions, from diabetes to heart disease, to gain insight into the difficulties they faced.
01
What difficulties do elderly patients experience managing their chronic conditions at home?
Going into our interviews, we expected to find that patients needed help with the technical elements of their treatment, such as medication management. However, behavioral and lifestyle changes, such as dietary and exercise, were the most difficult to implement. It is due to the long-established diet and physical activity preferences of elderly patients that negatively affected their commitment to sticking to their physician’s recommendations. We discovered many elements are out of the patient's control, influencing the maintenance of their treatment plans. These included environmental elements (ex., proximity to grocery stores), social elements (ex., proximity to family who can help), and the effects of aging (ex., declining cognitive abilities).
"When the weather is not good, or the day is busy with meetings, or the gym is too far from my home, I don't want to do something similar because the physicians themselves don't exercise as my physician told me to."
- Patient 3
Key Insight: It is important to consider a patient’s personal lifestyle goals and medical goals to develop personalized roadmaps.
02
What difficulties do elderly patients experience with communication with their physicians?
Many patients feel they lack connections to others going through a similar experience. They sometimes feel that their doctors do not understand from an emotional and mental viewpoint because they have not personally experienced the disease. In addition, when patients receive treatment plans, they often focus solely on achieving the necessary medical goals to combat the disease. However, it is important to consider the patient’s lifestyle goals to influence and motivate them. This holistic approach is more relevant and motivating to patients.
"The problem of communication in medicine is that it often focuses on clarity, not discussion or persuasion. Doctors need to understand what works for patients and what motivates them to actually do it."
- Subject Matter Expert 1
"I wish I had someone to talk to who had been through it and knew how it feels or how scary it is. They have the knowledge but haven't experienced the disease themselves."
- Patient 2
Key Insight: Patients desire to connect to a patient community for support and advice and want their voices to be heard.
03
What strategies and resources do elderly patients currently utilize for at-home treatment management for both medical (medications) and lifestyle changes (exercise/diet)?
Patients value their independence. Many factors, including their physical, mental, and financial capabilities, contribute to this. In addition, many patients prefer to manage their health independently without the help of others. This demonstrates the importance of personalized treatment plans to a patient’s contextual situation. Patients receiving their treatment plan may include instructions such as taking medication and exercising. However, these instructions often do not consider the patient’s environmental and social context, which can influence their ability to implement these changes.
"Wellness is different from healing. Wellness is what and how you want to live your life. How do I want to live, and what is that going to require me to do, and how do I continue on."
- Subject Matter Expert 2
Key Insight: A patient’s environmental and social context influences their daily routine, which can affect the management of their treatment plan.
04
What are the current alternative care models within the healthcare industry?
We analyzed existing alternative care models to understand better how they are trying to intervene within the current healthcare space. We compared the alternative care models to the common care model to understand both systems' pros and cons. We looked into 32 examples and observed four main types of alternative models: (1) Telehealth, (2) Micro Hospitals, (3) Home Visits, and (4) Internet-based care.
Key Insight: The current medical practices are disjointed, which restricts and inhibits opportunities to obtain a holistic picture of the patient.
Design Imperatives
Based on our exploratory research, we developed a framework for our solution using six design imperatives. Each is based on observations and insights gleaned from in-depth interviews and secondary research.
Humanistic
Facilitate human interaction and help patients build supported bonds
Positive
Project a tone within interactions that will influence a positive attitude within patients
Voluntary
Project a tone within content that encourages voluntary participation
Personalized
Adapt to personal needs and context and provide control and autonomy for patients
Streamlined
Ensure each touchpoint builds on one another to help patients feel their voice is heard
Simple, Natural Interactions
Reduce cognitive load for elderly patients with cognitive and mobility impairments
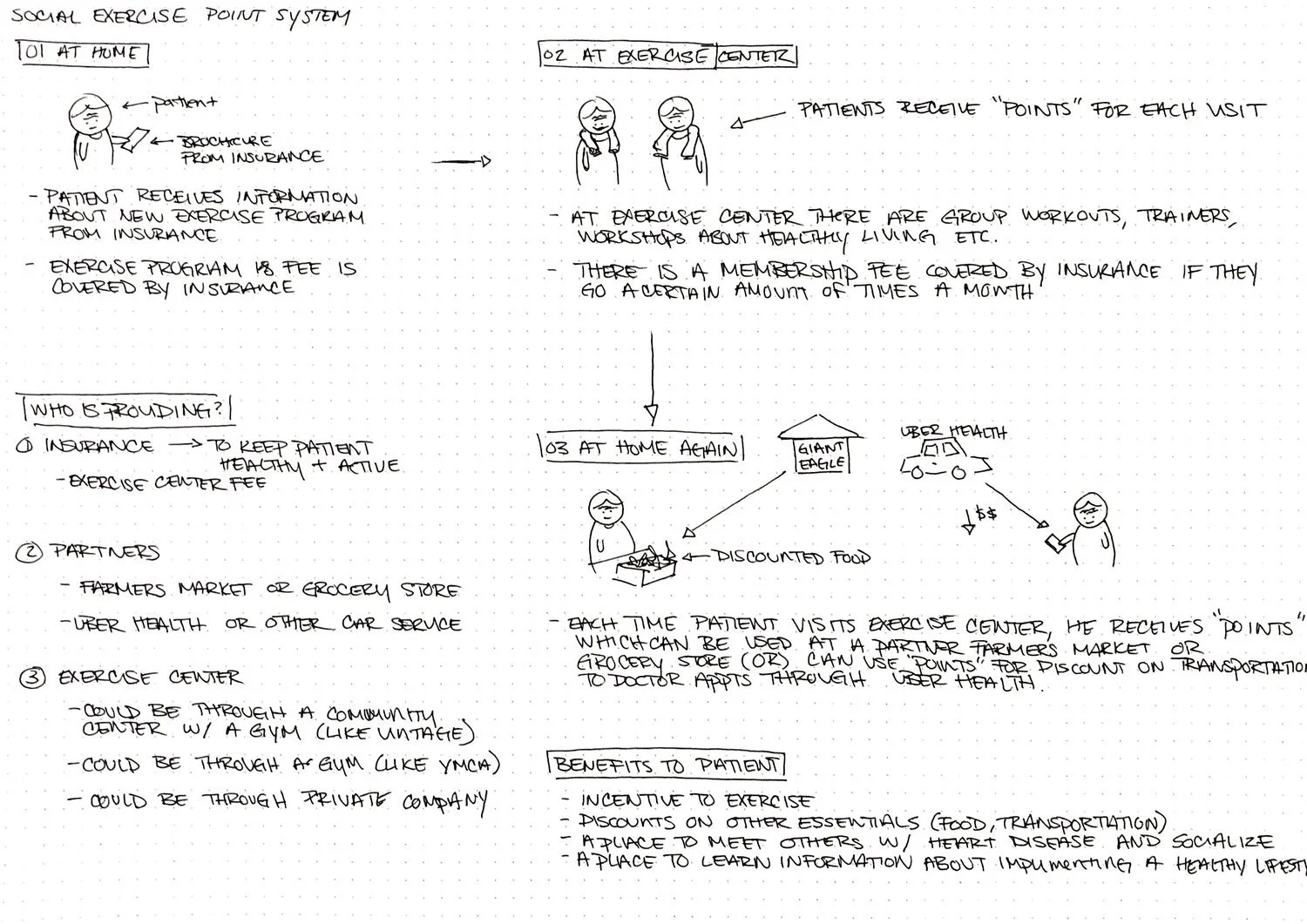
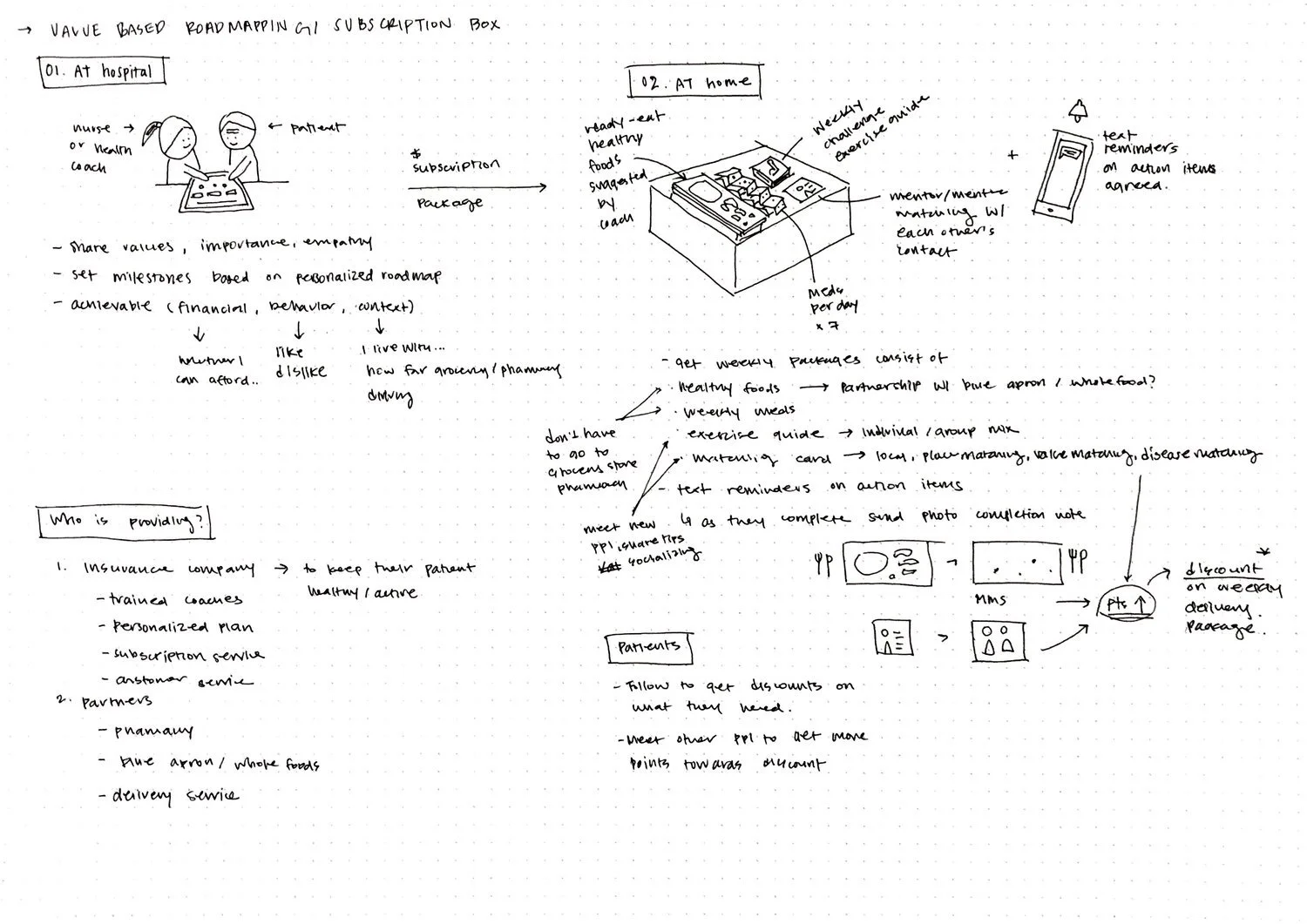
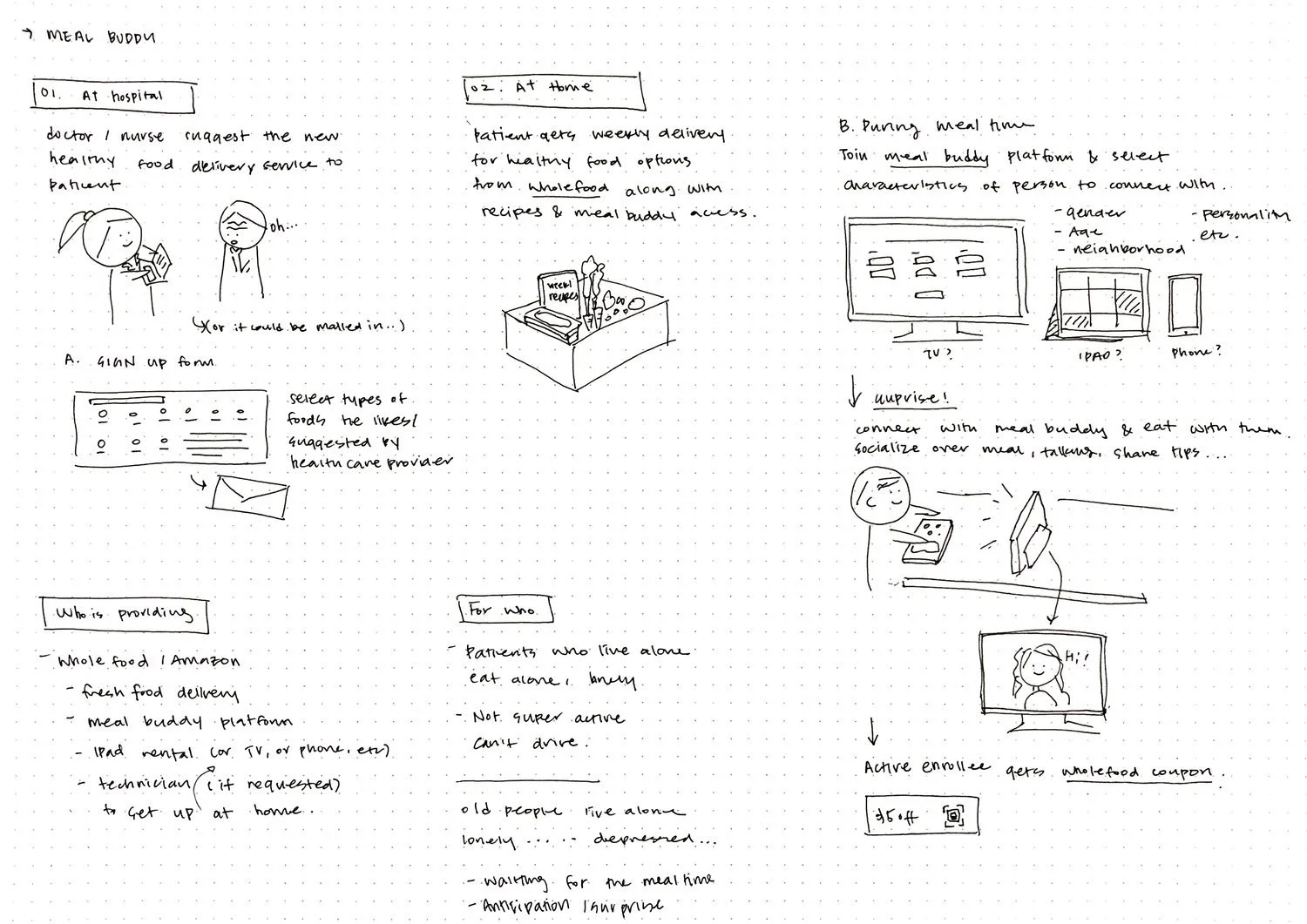
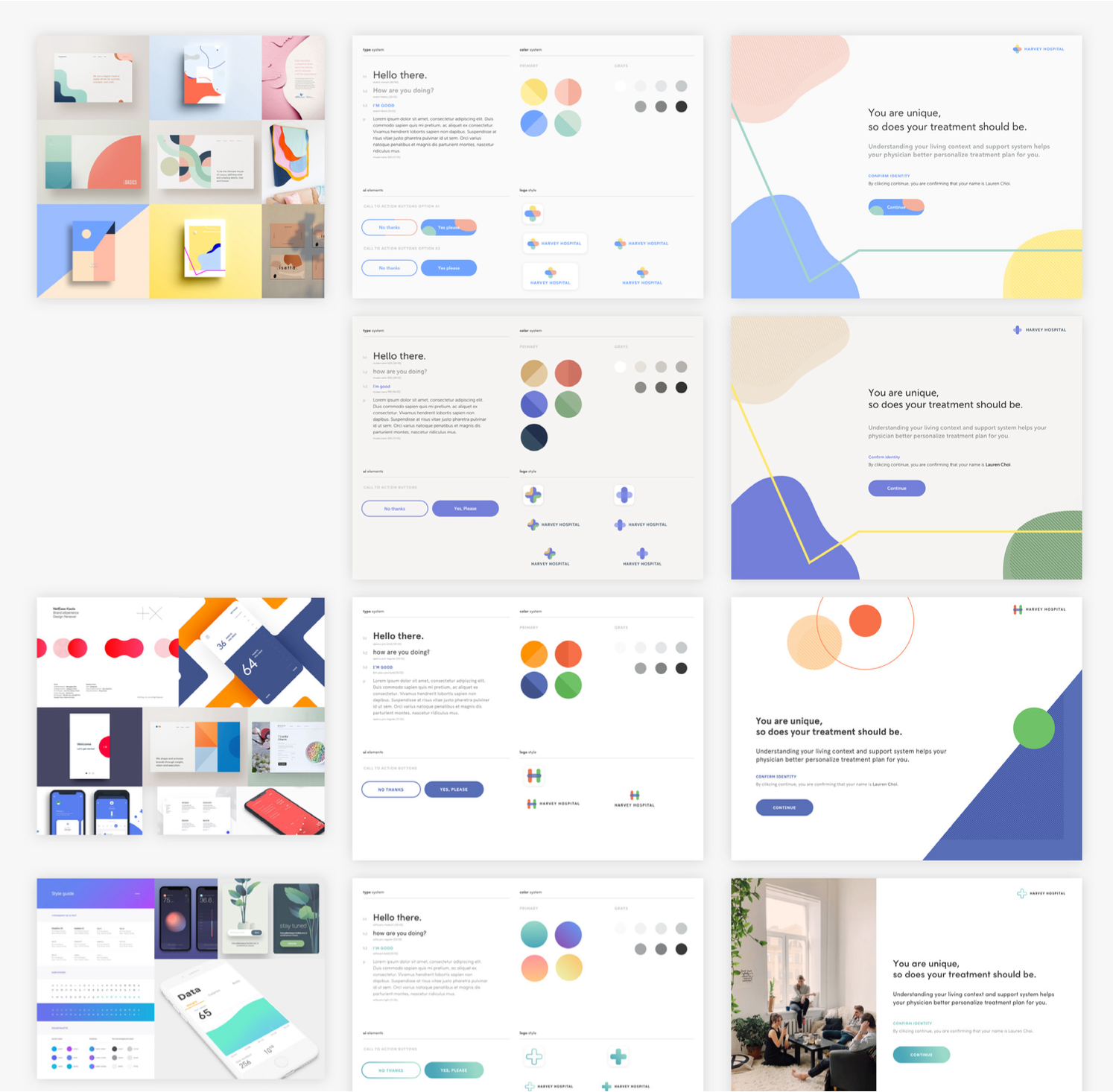
Design Exploration
During our concept ideation process, we focused on providing as many resources as possible within our ideas and initially focused on at-home treatment adherence solutions. We explored concepts around 4 main topics: (1) Behavioral support, (2) Resource management, (3) Communication support, and (4) Community support. We tested our concepts at the local community center for seniors.
Feedback
Seniors emphasized the importance of in-person relationships with their doctors, desired support with access to narrowed and personalized information and reducing administrative complexity, and building connections with outside support systems, who act as surrogate families to them.
Pivot
While initially focusing on at-home solutions, we decided to shift our focus to addressing interactions within the office environment based on the feedback we received. We did this based on two factors we discovered from speaking with elderly patients:
Seniors had strong views of healthcare being associated with their doctors and the interactions within the office environment.
Communication and bedside manner greatly influenced the patient's receptiveness to the doctor's recommendations.
By directly targeting elderly patients' current perceptions of health and designing opportunities to gain a more holistic understanding of patients within the office environment, physicians can provide better care for them, influencing at-home treatment adherence.
Value Proposition
As we moved through final concept development and prototyping, we outlined the value of the care ecosystem to understand how each proposed touchpoint relies closely on collecting meaningful patient data.
The point-of-time and data transfer method allows the physician to better understand the patient at the right time and personalize the communication approach and treatment plan. Moreover, cumulative data collection helps build a comprehensive patient profile to support patients outside the clinical environment and increase their autonomy in managing their conditions.
Reflections
This project was an exercise in developing a complete project, from topic selection to in-depth research and developing a design outcome. Because of the scope of our design concept, we did not have the opportunity to user-test the flow of our service and focused on testing the individual touchpoints. We need to test the service flow through prototyping for the next steps.
For future studies, it would be worth further looking into the following:
Al & Personalization: Examine how big data and algorithms can provide insights into patients' lives outside of the hospital environment.
Automation & Documentation: Examine how emerging technology, such as speech recognition and natural language processing, can aid the physician documentation process to enable physicians to focus on patient conversations during the examination fully.
Staffing and Training: Human interaction plays a significant role in patient experience. Examine the roles of care staff and determine how staffing and appropriate training should be administered.
Voice User Interface: How can a conversational interface be utilized for more natural interaction in the home environment to answer medical questions and collect patient information?