Opening communication and awareness about the impacts of chronic pain
Challenge
To explore the communication and visualization of chronic pain between patients, doctors, and family/friends and examine the reasons for poor communication to design an intervention that focuses on the mental and social aspects of patients’ experience and how patient self-awareness and family education could improve open communication.
Duration
16 weeks
Role
Designer & Researcher
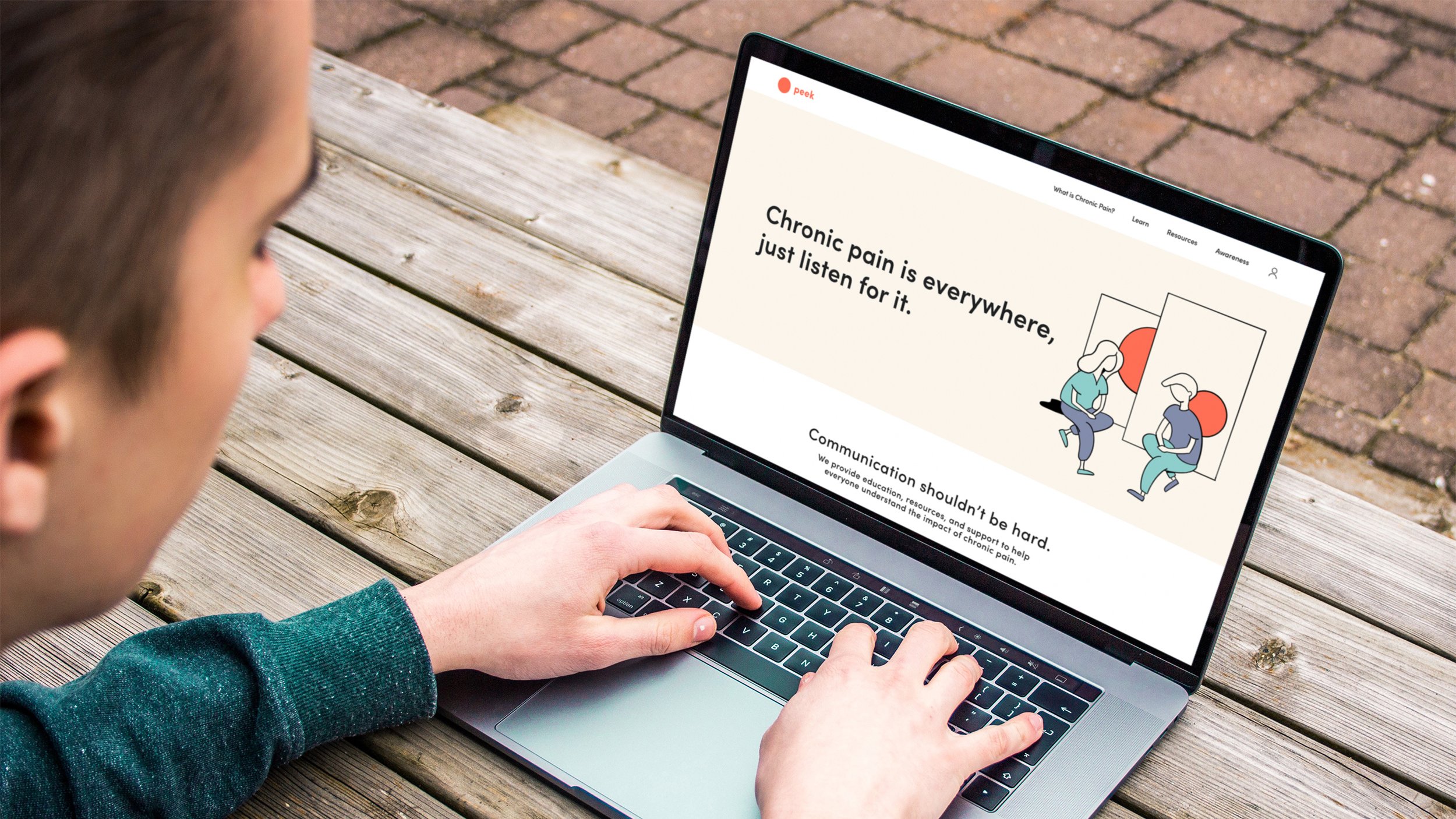
Peek
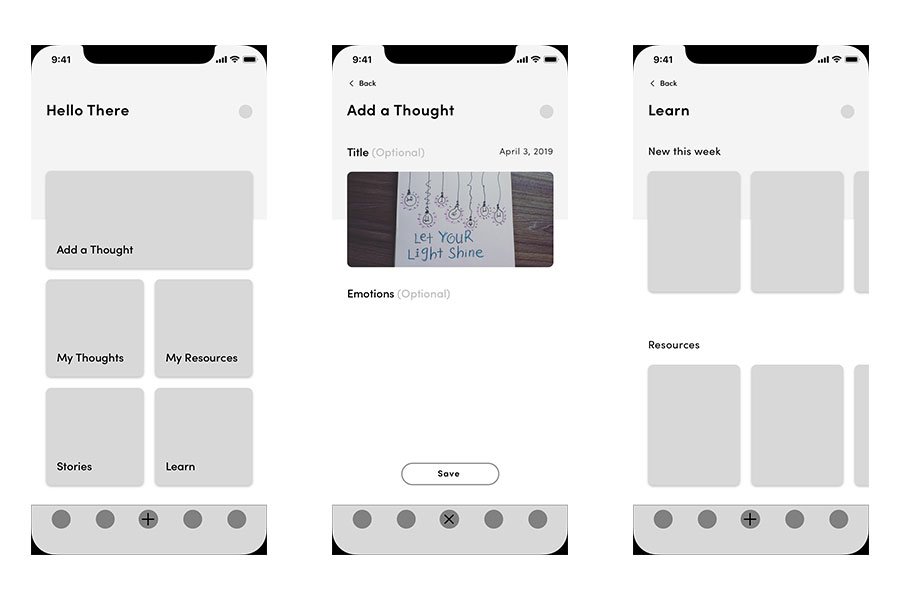
Peek is an online platform that focuses on spreading awareness of the mental, emotional, and social impacts of chronic pain. It features resources centered around communication and understanding that are helpful for both chronic pain patients and their families and friends.
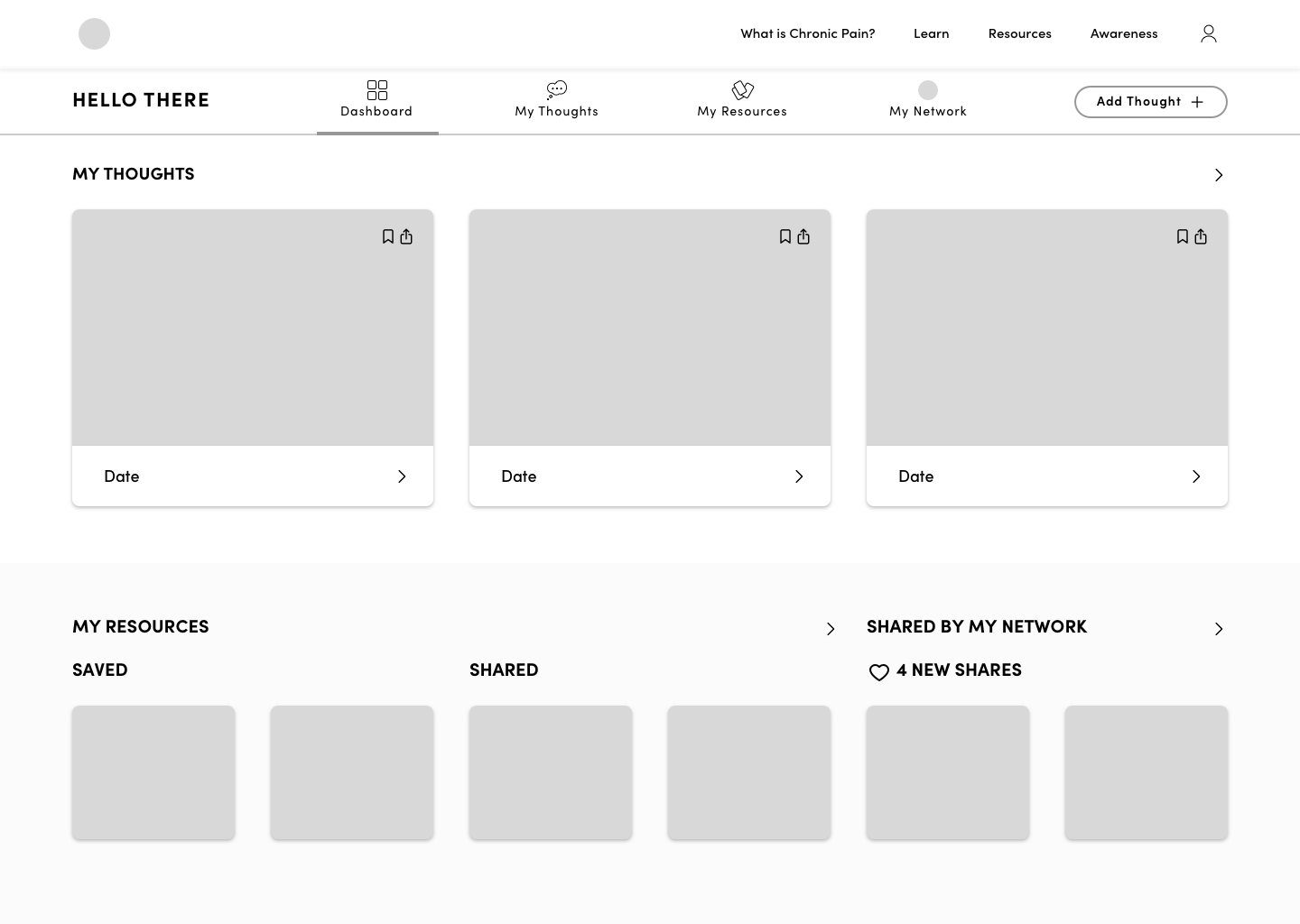
Peek has two main elements: (1) The website features free resources, information, and shared stories that are accessible without signing up. (2) The platform is a resource to help chronic pain patients and their family/friends record their thoughts, build a collection of resources, and share them.
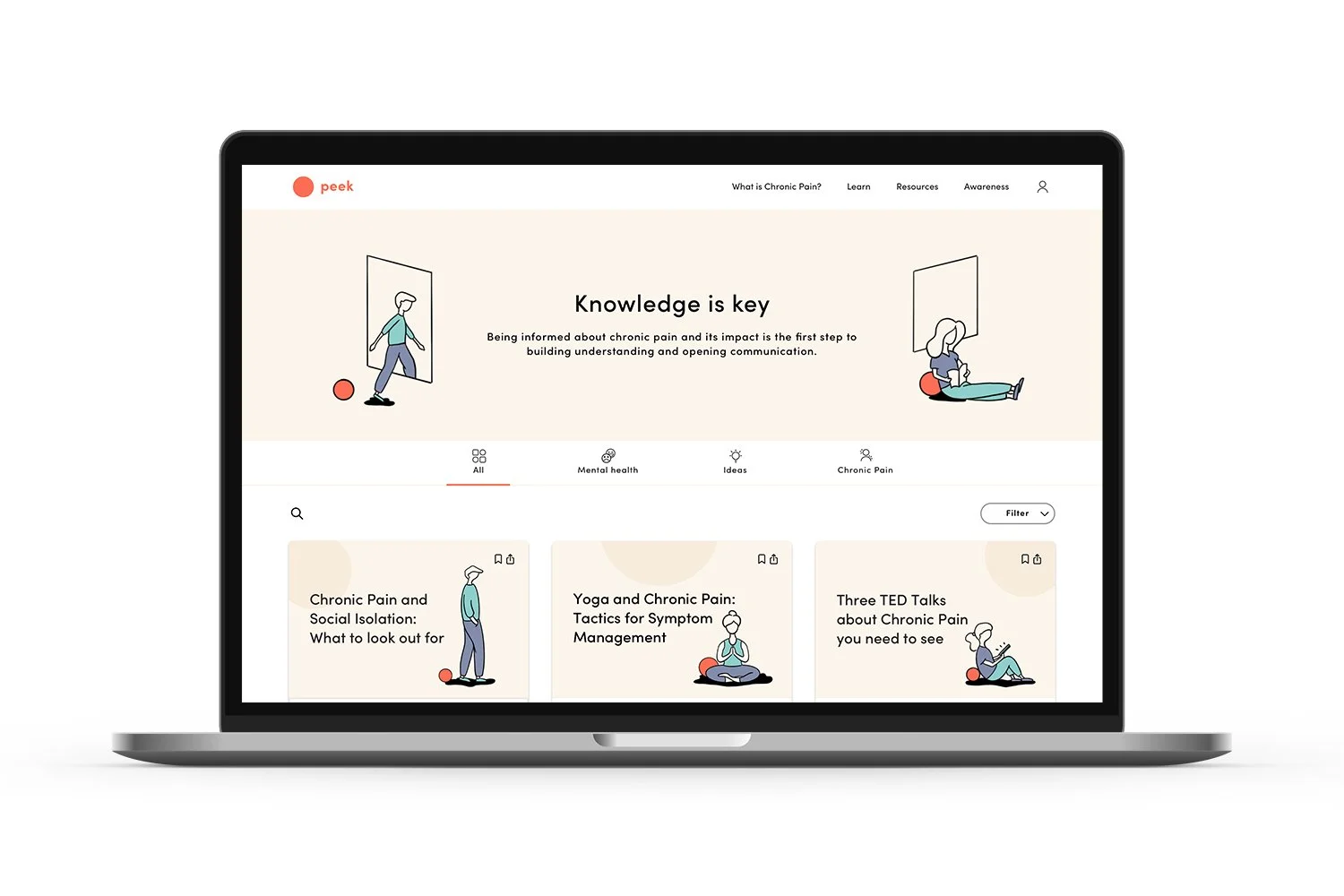
Learning to Build Understanding
The Peek website features public articles about chronic pain, its mental effects, and ideas/perspectives about chronic pain. This is the first step in building understanding and opening communication around chronic pain.
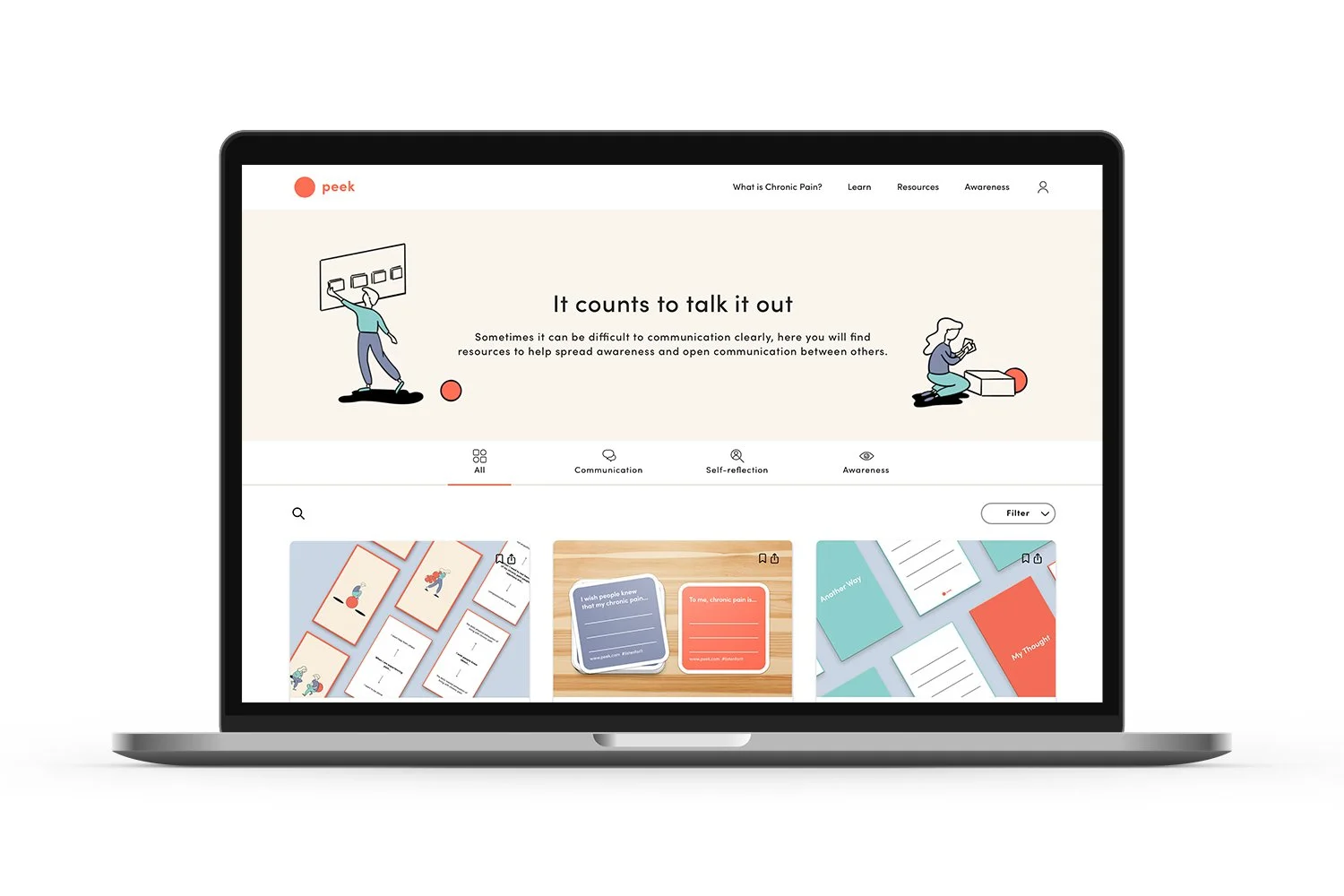
Resources to Open Communication
The Peek website features free downloadable resources for the public that facilitate open communication, self-reflection, and promoting awareness.
Inspired by design research methods, these resources focus on raising questions and providing a starting point for conversations through individual or group exercises.
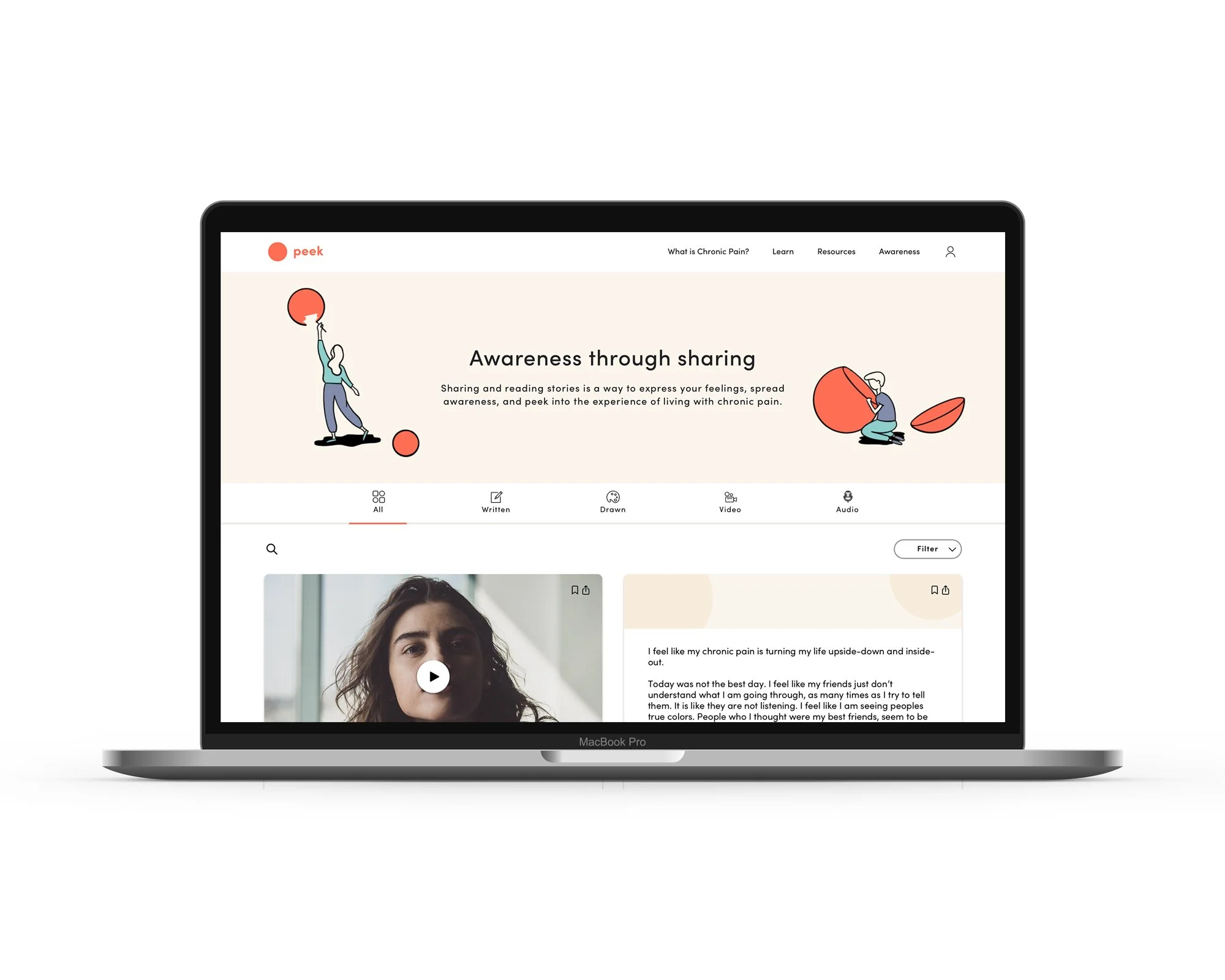
Awareness by Sharing Experiences
Users can read publicly shared thoughts and stories from the Peek network. These stories are shared voluntarily by Peek users and aim to spread awareness, build empathy, and help people see how chronic pain affects others.
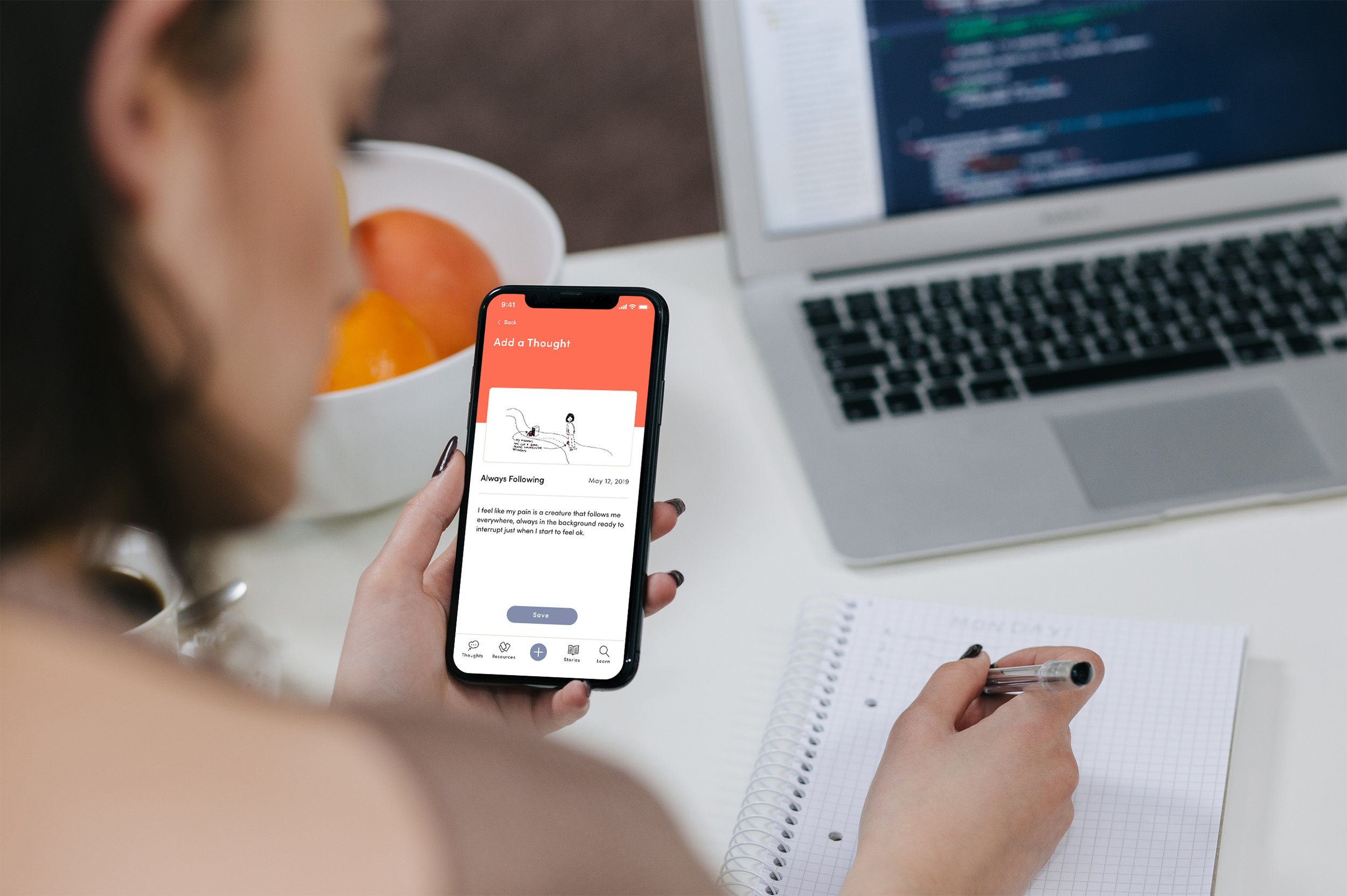
Timeline of Thoughts
The Peek platform allows users to chronicle their thoughts over time, providing a unique approach to managing chronic pain's mental/emotional impacts.
This collection of thoughts and experiences becomes a powerful resource, enhancing communication about their chronic pain journey. For instance, they can share a video with their doctor, a medium that may convey their experience more accurately, capturing their body language and expression in the moment rather than relying solely on verbal recall.
Multiple Methods of Expression
Users can write, draw, video, or audio record their thoughts. Many chronic pain patients have difficulty describing their pain when recalling it to others. Using different media, the user can select the one that best represents the thought they are trying to express at that moment.
For example, some may prefer audio recording because it allows the tone and emotion within the voice to be heard at that moment.
Sharing to Open Communication
Users can share resources and thoughts with their family and friends in the Peek network and vice versa.
By seamlessly sharing thoughts and resources, the patient and their family/friends can start understanding each other's perspectives and feelings and build open communication channels.
Exploring the Root of the Thought
The user can further explore their thoughts through additional questioning.
Based on "The Five Whys," the process would start with a significant part of the thought. It would prompt the user with a question related to that statement. From there, they would use their answers to continue thinking through the thought. It would end with an overview and a prompt to think of an alternative way to think about the original statement.
So, how did I get here…read more about the process below
The Big Question
How might I bring awareness to the mental and emotional impact of chronic pain to improve patient self-awareness and open communication with family, friends, and the public?
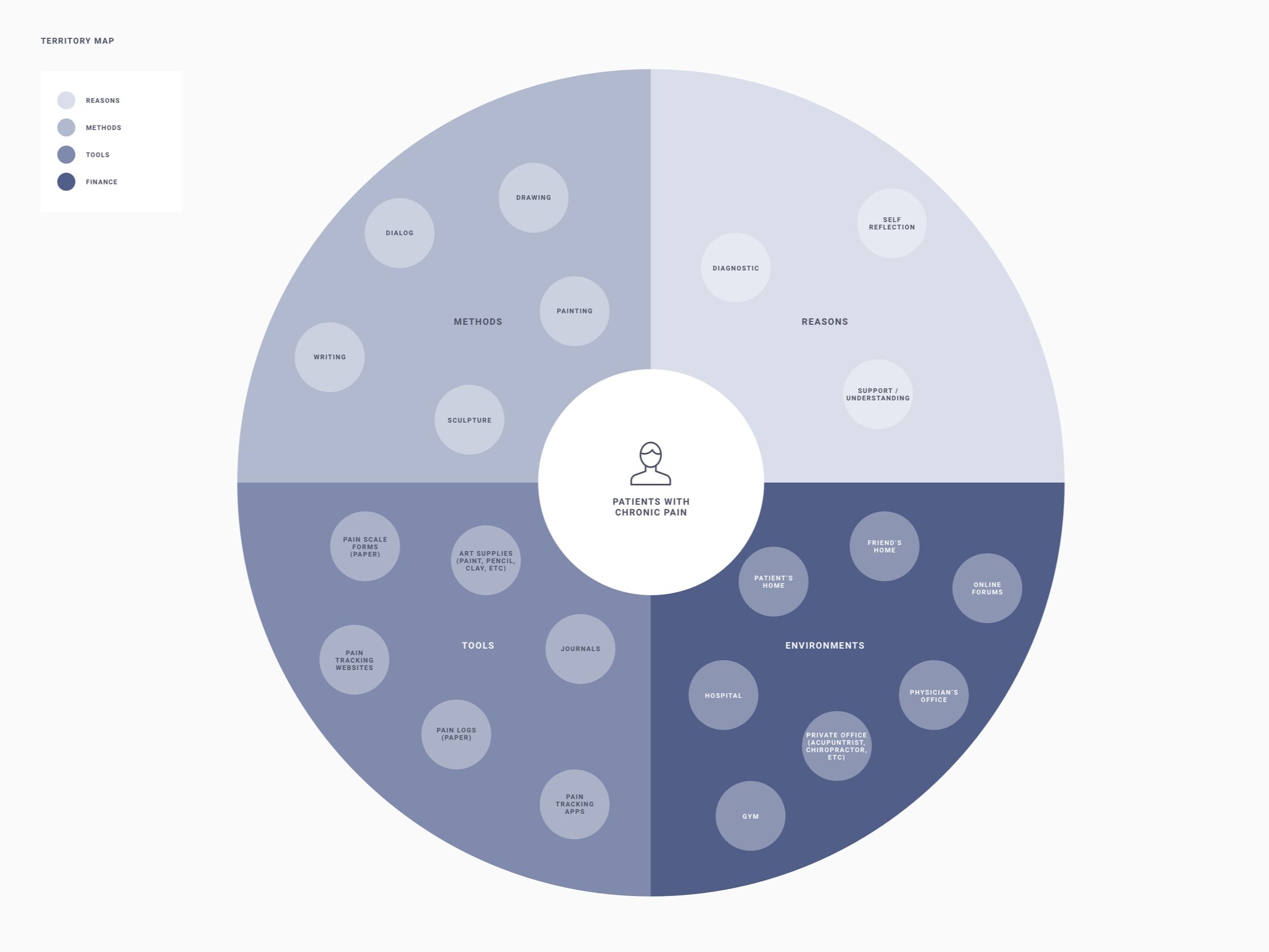
Research
To tackle this challenge, I conducted market research and in-depth interviews and utilized online patient forums to understand the patient experience and perspective. I broke down my initial questions to help me contextualize the experience of chronic pain patients and understand the difficulties they experienced communicating with their doctors, family, and friends.
01
How does communication differ for a patient with chronic pain when speaking with a medical professional vs a family member or friend?
Many patients feel they lack connections to others going through a similar experience. They tend to focus on the physical symptoms with their doctors because they directly impact them and are looking for solutions to manage them. However, when interacting with family and friends, they rarely share their experiences because they do not think they can relate to the mental experience, cannot provide any help with the physical symptoms, or make them uncomfortable.
" I find whenever I do start talking about it (the pain), it makes people uncomfortable."
- Participant 2
"The pain gets to your spirit, and you become different. And isolated. Like me, I have isolated myself."
- Participant 5
Key Insight: Patients do not share with their family and friends because they do not think they can help them with the physical symptoms.
Key Insight: Patients find dealing with daily pain as mentally exhausting. They do not believe their family/friends can understand or believe the degree of mental exhaustion they experience.
02
What are the current strategies patients with chronic pain use to communicate how their pain feels to medical professionals, family, and friends?
The major of communication is verbal when describing pain to doctors and family/friends. Existing solutions used within medical environments include numerical rating scales, visual analog scales (ex., Wong-Baker Faces Pain Scale), and categorial scales (ex., McGill Pain Questionnaire). Many of these focus on the physicality of pain. Additionally, symptom tracker apps, such as Wave and Bearable, focus on tracking symptoms and monitoring activities to identify trends. Some of these capture chronic pain's mental, emotional, and social impacts. However, it is still up to the patient to contextualize it verbally with their doctors.
Key Insight: Patients focus on strategies for physical symptoms because they experience them more directly and are easier to articulate.
03
What are their current perceptions of how chronic pain is perceived in society, and how does that impact their willingness to talk about their chronic pain experiences?
Many patients view their chronic pain as a private experience, mainly because it is an invisible disease to the general population. Many patients feel the general population relates pain to the image of an individual experiencing acute pain, as it is something that can be seen or they have personally experienced. This can result in patients developing a fear of becoming a burden, not asking for help because of people’s perceptions, and even self-isolation over the long term.
"Most people have a mental picture of people living with pain as being completely unhealthy, in a wheelchair, with a walker; the picture that society has painted of people with pain is sad."
- Participant 3
"It is a very private experience. It is not like anyone is listening."
- Participant 3
"As open as I am talking about the pain, I never ask for help mostly because I don't want to burden someone else, but in a way, having help would be really beneficial."
- Participant 4
Key Insight: Patients see their pain as a private experience because no one can see it resulting in lack of communication with others.
Key Insight: Patients are aware they have isolated themselves; however, they find it easier to avoid than to explain.
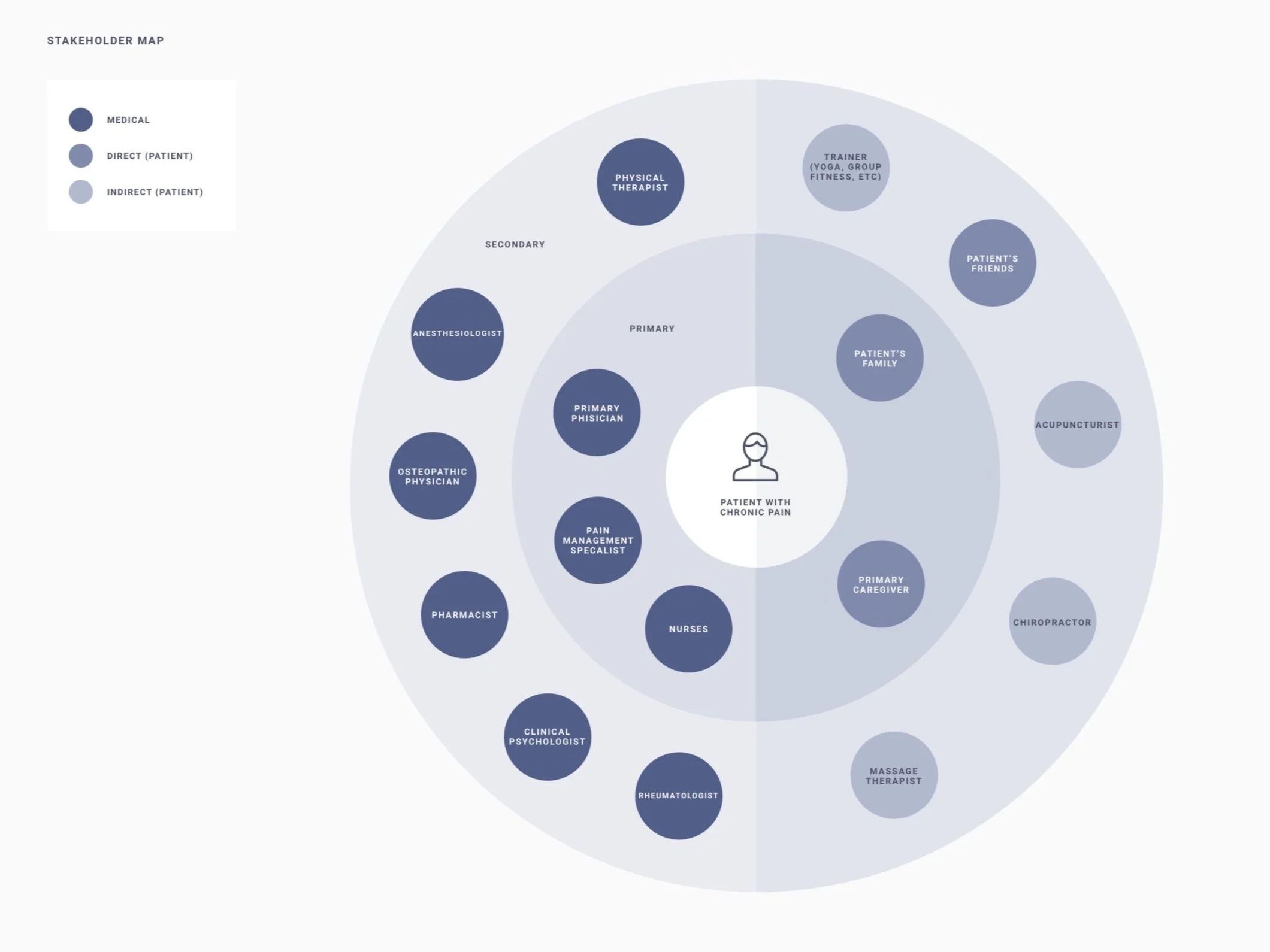
Focusing on Patients and their Family and Friends
Based on my exploratory research, I focused on fostering communication between patients and their family/friends. This was based on two main factors:
Patients are less likely to talk about their chronic pain with family and friends. Patients may actively avoid social situations where their chronic pain will be an issue.
Lack of communication and avoidance leads to patients isolating themselves from others, which affects personal relationships and potential support systems that could benefit the patient.
While family and friends can not impact how a patient manages the physical symptoms, they can be a resource for providing mental and emotional support. By improving open communication, where the patient and family/friends are aligned and educated on one another's perspectives, experiences, and feelings early on, there is an opportunity to prevent the isolation common among patients with chronic pain.
Design Imperatives
Based on my exploratory research, I developed a framework for our solution using four design imperatives. Each is based on observations and insights gleaned from in-depth interviews and secondary research.
Foster Engagement
Provide resources for patients and family to engage in discussion
Encourage Self-Reflection
Encourage patients and family to reflect on their actions and thoughts to promote thoughtful communication
Encourage Critical Thinking
Encourage patients and family to observe their actions and thoughts from a critical lens
Flexibility in Communication
Provide the patient with multiple methods of communication for personalized expression
Design Exploration
With the core problem being the lack of open communication between patients and family members, I explored three main concepts: (1) Connected Educational Resources, (2) Challenging Negative Thoughts, and (3) Expression Toolkits. I moved forward with the expression toolkits and public awareness campaign. I further refined the concept and explored low-cost solutions to make it available to many users.

Reflections
This project was an exercise in developing a complete project, from topic selection to in-depth research and developing a design outcome. For the next steps, I plan to speak with pain specialists and chronic pain patients about the viability of the high-level concept.
For future studies, it would be worth further looking into the following:
Al & Personalization: Examine how big data and algorithms can provide insights into patients' mental and emotional trends, provide targeted recommendations, and support patients in utilizing media methods they may not be comfortable with, such as voice-to-image.